Type 2 diabetes: Symptoms, causes and treatment
Type 2 diabetes is a condition characterized by high blood sugar (glucose) levels.

The most common form of diabetes, type 2 diabetes is a chronic disease whose defining factor is high blood sugar, or glucose.
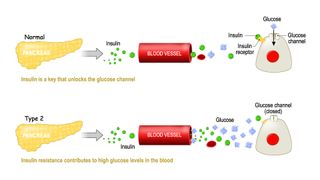
Glucose is a critical source of energy for the body's cells. When someone eats food, any of the sugars in that food ultimately enters the blood; then, the pancreas releases the hormone insulin, which guides the blood glucose into cells. That step is essential to keeping the body’s cells fueled and also maintaining a healthy level of glucose in the blood.. However, in people with type 2 diabetes, the pancreas doesn't produce enough insulin and/or the body doesn't use that insulin efficiently.
The result is an elevated level of glucose in the blood, which, over time, can lead to a host of serious complications, including heart disease, kidney disease and eye disease.
More than 37 million people in the U.S., or roughly 1 in 10, have diabetes, according to the Centers for Disease Control and Prevention (CDC); of those, about 90% to 95% have type 2 diabetes.
In addition, about 96 million people in the U.S., or about 1 in 3, have prediabetes, in which blood sugar levels are high but not high enough for a person to be diagnosed with type 2 diabetes, per the CDC. This condition puts them at risk for diabetes, heart disease and stroke, but most are unaware they have it.
Causes
Type 2 diabetes is linked to both genetic and lifestyle factors. Risk factors include having prediabetes, being overweight, engaging in less than 150 minutes of exercise a week and being older than 45, the CDC says. The disease also tends to run in families and occurs more often in African American, Hispanic/Latino American Indian and Alaska Native populations.
Why these factors raise the risk of the chronic disease is unclear. One possible link, according to the National Institute of Diabetes and Digestive and Kidney Diseases, involves extra weight, particularly around the waist. Extra fat has been linked to insulin resistance, in which the body does not use insulin efficiently to regulate blood sugar. Though researchers aren’t certain the mechanism behind this link, according to the American Diabetes Association, that extra fat could lead to inflammation, physiological stress or other changes in the body’s cells that ultimately cause insulin resistance. Notably, however, type 2 diabetes can also develop in people who are not overweight or obese, mostly in older adults.
Symptoms & complications
Early symptoms of type 2 diabetes include increased thirst, urination and hunger; fatigue; blurred vision; tingling extremities; and slowly healing sores or skin infections, according to the National Library of Medicine. But these symptoms often appear gradually over the course of years and can be so mild that they are missed. Sometimes, there are no symptoms at all.
Unexplained weight loss can also be a symptom of type 2 diabetes, said Dr. Minisha Sood, an endocrinologist at Northwell Health in New York. This symptom can sometimes be confusing to patients, because diabetes is associated with obesity and too much weight gain. And although this is true, type 2 diabetes can lead to weight loss, mostly through a decrease in "water weight," she said.
"When blood sugar exceeds a certain level … the body has to eliminate that sugar somehow," Sood said. This is done mostly through the kidneys, and the body also gets rid of water along with the sugar. "Patients end up losing a lot of water," she said.
The long-term complications of type 2 diabetes include heart attack, nerve and kidney damage, blindness, erectile dysfunction and dementia, according to the Cleveland Clinic. For instance, having too much glucose in your blood can lead to eye diseases such as diabetic retinopathy, which affects blood vessels in the retina and is the leading cause of blindness in the U.S.; glaucoma, which in the case of diabetes can result from damage to blood vessels in the front of the eye that ultimately causes fluid build-up and damage to the optic nerve; cataracts, which tends to develop more readily in someone with diabetes, possibly due to deposits of glucose in the eyes' lenses, according to Medline Plus.
Although these complications may seem varied, there is a common link. "Glucose can be toxic to blood vessels," Sood said, and damage to blood vessels over time causes some of these serious conditions.
COVID-19, the disease caused by the coronavirus SARS-CoV-2, can also be more serious in individuals with diabetes compared with people who don’t have diabetes. For instance, research published April 23, 2020 in the Journal of Infection, suggested people with diabetes were 3.7 times more likely to have a severe case of COVID-19 or to die from it as compared with individuals with no underlying health conditions. That research was based on a review of 13 relevant studies.
There is also preliminary research suggesting that COVID-19 can cause both type 1 diabetes and type 2 diabetes. In a study based on information from two health databases, researchers found that individuals younger than 18 were more likely to be diagnosed with diabetes more than 30 days after a COVID-19 infection compared with individuals not infected with the disease, researchers reported online Jan. 14, 2022 in the CDC journal Morbidity and Mortality Weekly Report. Diabetes diagnoses in these COVID-19 patients were 166% and 31% greater compared with non-COVID-19 individuals, respectively for the two databases.
Diagnosis
Some people learn they have type 2 diabetes through routine blood testing — for example, when a doctor checks blood glucose levels during an annual exam, or for diabetes screening, Sood said.
The American Diabetes Association recommends screening for all adults age 45 and older, as well as in the following groups, the Mayo Clinic reported:
- Individuals who are under 45 and who are overweight or have obesity, plus have one or more risk factors tied to diabetes.
- Women who have been diagnosed with gestational diabetes.
- Individuals with a prediabetes diagnosis.
- Kids who are overweight or have obesity, plus have a family history of type 2 diabetes or one or more other risk factors.
Though normal blood sugar levels can vary among individuals, there are certain ranges that are considered "normal." For instance, fasting blood sugar (the amount of glucose in the blood at least eight hours after a meal) is between 70 and 100 milligrams per deciliter (mg/dL), according to the World Health Organization (WHO). Most people's blood glucose levels rise after they eat. According to the American Diabetes Association (ADA), the normal blood sugar range two hours after someone eats is generally less than 140 mg/dL.
According to the ADA, a person can be diagnosed with diabetes if they meet one of these criteria:
- They have a fasting blood glucose level greater than or equal to 126 mg/dL.
- They have a blood glucose level greater than or equal to 200 mg/dL two hours after they drink a special sugar solution.
- They get a result of greater than or equal to 6.5% on an A1C test, which measures average blood sugar for the past three months, roughly.
Given that a family history of type 2 diabetes raises the risk of developing the condition, people who fall into that category should talk to their doctor about being screened, Sood said.
"If it's screened for, and identified early, changes can be implemented that could prevent progression of the disease, and complications," Sood told Live Science.
Treatment
To manage type 2 diabetes, doctors recommend changes to your diet. Eating a healthy including smaller portion sizes; increased intake of high-fiber foods, such as fruits, non-starchy vegetables and whole grains; and fewer calories — and getting regular exercise, the Mayo Clinic says. A keto diet may also be a potential way for diabetics to manage their condition.
Doctors also may prescribe insulin, other injectable medications, or oral diabetes medicines, such as metformin, to address the high blood sugar. Metformin works by both reducing the amount of glucose produced by the liver and increasing the body’s sensitivity to insulin (to become less insulin resistant), according to the diaTribe Foundation. Patients are typically given blood sugar targets and are advised to check their glucose levels periodically.
For people who have obesity and type 2 diabetes and who also have trouble controlling their blood sugars with these treatments, weight loss surgery, also called bariatric surgery, can be a last resort option, according to the National Institute of Diabetes and Digestive and Kidney Diseases. However, the long-term results of this surgery are still being studied.
In 2016, the U.S. Food and Drug Administration approved the use of an "artificial pancreas" that automatically tests blood glucose levels periodically and releases insulin accordingly, Live Science previously reported.
For people who are diagnosed with type 2 diabetes and have weight issues, Sood recommends they lose at least 5% to 10% of their current body weight. If lifestyle changes don't work well enough to get a person's blood sugar levels under control, then doctors generally prescribe medications to complement those changes, she said.
Is there a cure for type 2 diabetes?
Type 2 diabetes is a progressive disease. New research now suggests that in some cases patients can go into remission, in which their blood sugar levels fall into normal range. Sustained weight loss has proved to be especially successful.
For instance, in the Diabetes Remission Clinical Trial in the U.K., researchers placed individuals with type 2 diabetes on a calorie-restrictive diet for a year, they reported Oct. 2, 2018 in the journal Cell Metabolism. Out of the 58 patients that stuck with the trial, 69% reached blood glucose levels (measured with the A1C test) that were in the non-diabetic range, meaning they would be classified as “in remission,” after they had lost weight; at the end of the 12 months, 64% showed non-diabetic blood glucose levels, the researchers reported. On average, those who responded to the treatment lost 35.7 pounds (16.2 kilograms).
- Related: Keto diet vs low carb: what's the difference?
- Related: Type 3 diabetes: Symptoms, causes and treatments
In another study, detailed in 2019 in the journal The Lancet Diabetes & Endocrinology, researchers looked at 300 people in the U.K. with type 2 diabetes. The study is still ongoing, but so far, it's shown encouraging results. In the study, half of the participants stopped taking their diabetes medications and started on a diet replacement formula, after which food was gradually reintroduced; the other half of the participants received standard diabetes care. Two years later, more than a third (36%) of the people with type 2 diabetes who took part in the weight management program were in remission.
However, remission does not mean the diabetes is "cured." That's because blood glucose levels constantly change and if a person were to regain lost weight or revert back to lifestyles that were impacting those levels, their sugars could go back up again to diabetic levels, according to the National Institute of Diabetes and Digestive and Kidney Diseases.
This article is for informational purposes only and is not meant to offer medical advice.
This article was updated on April 11, 2022, by Live Science Contributor Natalie Grover.
Additional resources
- Learn about how having diabetes can affect pregnancy in this explainer from the National Institute of Diabetes and Digestive and Kidney Diseases.
- Check out the latest data on the rising incidence of type 2 diabetes in children and teens in this report by the CDC.
- Learn how blood sugar works and how to achieve blood sugar health in the book "Blood Sugar 101: What They Don't Tell You about Diabetes".
Bibliography
"Type 2 Diabetes," National Institute of Diabetes and Digestive and Kidney Diseases
https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-2-diabetes#diagnose
"Mean fasting blood glucose," World Health Organization https://www.who.int/data/gho/indicator-metadata-registry/imr-details/2380
"Symptoms & Causes of Diabetes," National Institute of Diabetes and Digestive and Kidney Diseases
https://www.niddk.nih.gov/health-information/diabetes/overview/symptoms-causes#type2
"Type 2 Diabetes" Centers for Disease Control and Prevention
https://www.cdc.gov/diabetes/basics/type2.html
"Prediabetes – Your Chance to Prevent Type 2 Diabetes," Centers for Disease Control and Prevention
https://www.cdc.gov/diabetes/basics/prediabetes.html
"Understanding A1C," American Diabetes Association
https://www.diabetes.org/a1c/diagnosis
"Diabetes: An Overview," Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/7104-diabetes-mellitus-an-overview
"Type 2 diabetes," The Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/diagnosis-treatment/drc-20351199
"Insulin, Medicines, & Other Diabetes Treatments," National Institute of Diabetes and Digestive and Kidney Disease
https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments
"Achieving Type 2 Diabetes Remission through Weight Loss," National Institute of Diabetes and Digestive and Kidney Disease
https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/achieving-type-2-diabetes-remission-through-weight-loss
"Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial," 2019 The Lancet
https://www.thelancet.com/journals/landia/article/PIIS2213-8587(19)30068-3/fulltext
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.